RPM Guide
A complete guide on how RPM (remote patient monitoring) can help your practice grow and why NXTSTIM is a better provider of the service.

What is RPM?
Remote patient monitoring (RPM), has gained significant traction within the medical community for two primary reasons:
- improved preventative, acute, and chronic care, and:
- the expansion of care beyond the confines of physical practices or hospitals.
The adoption of remote patient monitoring (RPM) has surged, particularly with the rise of telehealth, facilitating consultations with patients via phone or video tools. With advancements in technology, remote patient monitoring (RPM) enables providers to remotely monitor their patients’ vital signs and other medical data in real-time, using software and mobile apps that interface seamlessly with Bluetooth and wifi-enabled devices.
As the prevalence of chronic illnesses rises in the United States, including obesity, diabetes, and hypertension, RPM has become a vital component of patient care, aiding in the early detection and management of these conditions. Only with NXTSTIM’s EcoAI device clinics have the option for setting up remote patient monitoring (RPM) for pain management as well.
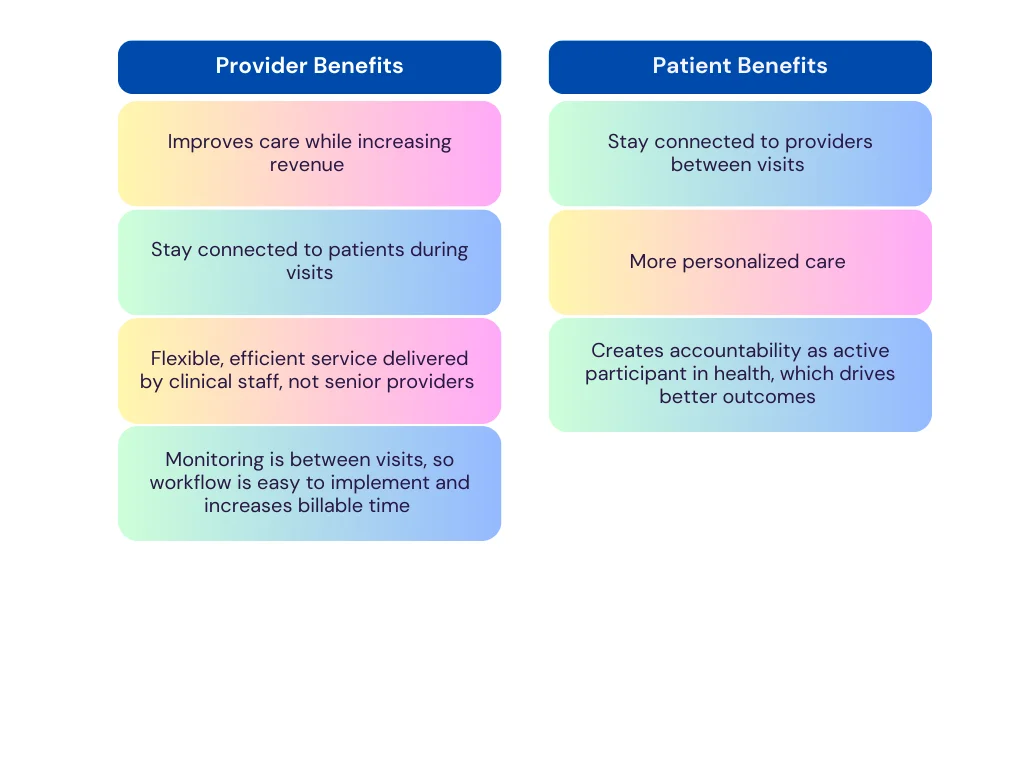
Benefits of RPM
RPM reduces patient visits while increasing revenue for clinics
In 2022 46% (https://www.cdc.gov/vitalsigns/health-worker-mental-health/index.html) of healthcare staff across the U.S. was recorded to have felt burnt out. With the ability to monitor patients remotely an average repeat patient can be counseled in a matter of minutes. Clinic staff is trained how to monitor patient data and can intervene by looking at it themselves or patients can contact them to understand any discrepancies in their health.
With RPM clinics can increase revenue in 2 ways:
- The reduction in visits also means that a clinic can increase the number of patients it treats, which in turn increases their revenue.
- Insurance codes that reimburse on setup, device supply and monitoring
Why choose NXTSTIM as an RPM partner:
After setup, the recording of data and CPT codes is a very intricate process and has 3 steps
- Monitoring
- Data Collection based on minutes monitored and CPT codes
- CMS guideline compliance
Monitoring
NXTSTIM’s smart dashboard has been designed to minimize the error, a mouse tracking system is installed into the dashboard. The mouse tracking system tracks the movement of the cursor when a designated RN monitors patient’s data and if the cursor remains stagnant for a while then the monitoring would not be counted. This system ensures that the monitoring recorded is exactly equal to the time an RN works on monitoring the data and meets CMS guidelines for conducting remote patient monitoring
CMS guidelines compliance
All monitoring done has to be recorded against the CPT codes for billing to be accurate. NXTSTIM’s smart dashboard automatically records the monitoring time against the codes, making sure that the data for the superbill is accurate.
Generating super bill
The superbill is generated automatically through our dashboard. This means that clinics that are affiliated with NXTSTIM do not have to worry about manually creating superbills after auditing data on monitoring each month.
CMS compliance for practices
FAQs
CPT Code 99457 allows for reimbursement for time spent by the billing physician, a qualified healthcare professional (“QHCP”), or clinical staff. All practitioners must practice in accordance with applicable state law and scope of practice laws.
The code requires the physician, QHCP, or clinical staff to spend at least 20 minutes per calendar month providing RPM services to a particular patient in order to receive reimbursement. Under this code it is required to have at least one live interaction with the patient.
- Approximate reimbursement amounts for each of the codes are as follows:
99453: $18.84 one time per episode of care*
99454: $48.93 every month
99457: $47.61 every month
99458: $38.68 every month if applicable
*NOTE: Amounts listed are approximate values only; reimbursement varies among MAC localities. Contact your local MAC to determine reimbursement amounts in your region.
The Remote Patient monitoring codes are not subject to the same restrictions that currently govern reimbursement of telehealth services under Medicare. Specifically, reimbursement for RPM services is not limited by geography to rural or medically underserved areas, nor is there any “originating site” requirement for RPM services. RPM services can be provided anywhere the patient is located, including at the patient’s home, or while out and about.
Private payers may reimburse for RPM services; however, they are not required to do so. It is important to note that private payers that do reimburse for RPM services may have different requirements for billing. Practitioners should check with the commercial payers in their region to determine whether services are reimbursable and what requirements must be met for billing.
Yes, for Medicare beneficiaries. As with other Medicare Part B services, RPM services are statutorily subject to a 20% beneficiary copay. With very limited exceptions, practices may not choose to waive the Medicare copay. Private payers may establish their own copays or may choose not to require a patient copay.
No. Practices should simply ensure that all requirements for each code are met (e.g. documenting patient consent for RPM services) and follow their current standard billing practices in submitting claims.
No. A practitioner may recommend RPM services for any patient whom s/he deems may benefit from some form of remote patient monitoring through improvements in care planning and treatments.
CPT Codes 99457 and 99091 are similar, but they differ in some important ways. CPT Code 99091 requires an aggregate of 30 minutes of time by a physician or QHCP during a 30-day time period, while CPT Code 99457 requires an aggregate of 20 minutes of time spent by clinical staff, physicians, or QHCPs during a calendar month. In addition, CPT Code 99457 requires live, interactive communication between the individual performing the services and the patient. A billing practitioner should carefully review the requirements for each and use his/her professional judgment to determine which code the provided services should fall under.
No. According to the CPT Code Manual, CPT Codes 99091 and 99457 cannot be billed for the same patient within 30 days of each other.
CMS does not set forth in the Final Rule a specific list of practitioners that are considered “Qualified Health Care Professionals” for purposes of these codes. The code descriptor for CPT Code 99091 references a qualified health care professional as “qualified by education, training, licensure/regulation (when applicable),” and this is the definition included in the American Medical Association’s CPT Manual. The AMA has indicated that the definition is drafted as intentionally broad so as to allow flexibility between payers, providers and regulatory agencies alike to determine the appropriate policies. When in doubt, consult your local Medicare Administrative Contractor (“MAC”).
CPT Code 99454 can only be billed once per patient each 30 days, regardless of whether the patient is using one device or multiple devices. Therefore, if a glucometer, a weight scale, and a blood pressure cuff are all provided to a patient for use in RPM and the devices meet all of the requirements for billing CPT Code 99454, the code could still only be billed once each 30 days for that patient.
